¡¡
¡¡
¡¡
Biochem J. 2002 Mar 1; 362(Pt 2): 507¨C512.
Dehydroascorbic acid uptake by coronary artery smooth muscle: effect of intracellular acidification.
Melanie E Holmes, James Mwanjewe, Sue E Samson, James V Haist, John X Wilson, S Jeffrey Dixon, Morris Karmazyn, and Ashok K Grover
Department of Medicine, McMaster University, Hamilton, Ontario, Canada L8N 3Z5.
ABSTRACT
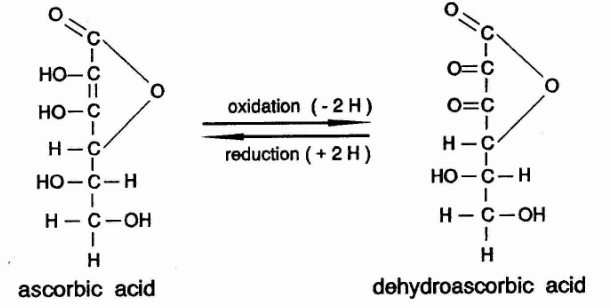
Dehydroascorbic acid (DHAA) enters cells via Na(+)-independent glucose transporters (GLUT) and is converted to ascorbate.¡¡
However, we found that Na(+) removal inhibited [(14)C]DHAA uptake by smooth-muscle cells cultured from pig coronary artery. The uptake was examined for 2-12 min at 10-200 microM DHAA in either the presence of 134 mM Na(+) or in its absence (N-methyl D-glucamine, choline or sucrose replaced Na(+)).
¡¡
This inhibition of DHAA uptake by Na(+) removal was paradoxical because it was inhibited by 2-deoxyglucose and cytochalasin B, as expected of transport via the GLUT pathway.
¡¡
We tested the hypothesis that this paradox resulted from an inefficient intracellular reduction of [(14)C]DHAA into [(14)C]ascorbate upon intracellular acidosis caused by the Na(+) removal.
¡¡
Consistent with this hypothesis: (i) the Na(+)/H(+)-exchange inhibitors ethylisopropyl amiloride and cariporide also decreased the uptake, (ii) Na(+) removal and Na(+)/H(+)-exchange inhibitors lowered cytosolic pH, with the decrease being larger in 12 min than in 2 min, and (iii) less of the cellular (14)C was present as ascorbate (determined by HPLC) in cells in Na(+)-free buffer than in those in Na(+)-containing buffer.
¡¡
This inability to obtain ascorbate from extracellular DHAA may be detrimental to the coronary artery under hypoxia-induced acidosis during ischaemia/reperfusion.
¡¡
Dehydroascorbic acid uptake by coronary artery smooth muscle: effect of intracellular acidification.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1222413/¡¡
¡¡
¡¡
SVCT1 and SVCT2: key proteins for vitamin C uptake
Vitamin C is accumulated in mammalian cells by two types of proteins: sodium-ascorbate co-transporters (SVCTs) and hexose transporters (GLUTs); in particular, SVCTs actively import ascorbate, the reduced form of this vitamin.
¡¡
SVCTs are surface glycoproteins encoded by two different genes, very similar in structure. They show distinct tissue distribution and functional characteristics, which indicate different physiological roles. SVCT1 is involved in whole-body homeostasis of vitamin C, while SVCT2 protects metabolically active cells against oxidative stress.
¡¡
Regulation at mRNA or protein level may serve for preferential accumulation of ascorbic acid at sites where it is needed.
¡¡
This review will summarize the present knowledge on structure, function and regulation of the SVCT transporters. Understanding the physiological role of SVCT1 and SVCT2 may lead to develop new therapeutic strategies to control intracellular vitamin C content or to promote tissue-specific delivery of vitamin C-drug conjugates.
(PDF) SVCT1 and SVCT2: key proteins for vitamin C uptake https://www.researchgate.net/publication/6293873_SVCT1_and_SVCT2_key_proteins_for_vitamin_C_uptake
¡¡
¡¡
Dehydroascorbic acid uptake by coronary artery smooth muscle: effect of intracellular acidification
¡¡
ABSTRACT
Dehydroascorbic acid (DHAA) enters cells via Na(+)-independent glucose transporters (GLUT) and is converted to ascorbate.
¡¡
However, we found that Na(+) removal inhibited [(14)C]DHAA uptake by smooth-muscle cells cultured from pig coronary artery.
¡¡
The uptake was examined for 2-12 min at 10-200 microM DHAA in either the presence of 134 mM Na(+) or in its absence (N-methyl D-glucamine, choline or sucrose replaced Na(+)). This inhibition of DHAA uptake by Na(+) removal was paradoxical because it was inhibited by 2-deoxyglucose and cytochalasin B, as expected of transport via the GLUT pathway.
¡¡
We tested the hypothesis that this paradox resulted from an inefficient intracellular reduction of [(14)C]DHAA into [(14)C]ascorbate upon intracellular acidosis caused by the Na(+) removal. Consistent with this hypothesis: (i) the Na(+)/H(+)-exchange inhibitors ethylisopropyl amiloride and cariporide also decreased the uptake, (ii) Na(+) removal and Na(+)/H(+)-exchange inhibitors lowered cytosolic pH, with the decrease being larger in 12 min than in 2 min, and (iii) less of the cellular (14)C was present as ascorbate (determined by HPLC) in cells in Na(+)-free buffer than in those in Na(+)-containing buffer. This inability to obtain ascorbate from extracellular DHAA may be detrimental to the coronary artery under hypoxia-induced acidosis during ischaemia/reperfusion.
¡¡
Melanie E Holmes, James Mwanjewe, Sue E Samson, James V Haist, John X Wilson, S Jeffrey Dixon, Morris Karmazyn, and Ashok K Grover
Department of Medicine, McMaster University, Hamilton, Ontario, Canada L8N 3Z5.
Author information Copyright and License information Disclaimer
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1222413/
¡¡
¡¡
Ascorbic acid depletion enhances expression of the sodium-dependent vitamin C transporters, SVCT1 and SVCT2, and uptake of ascorbic acid in livers of SMP30/GNL knockout mice.
¡¡
Arch Biochem Biophys. 2010; 496(1):38-44 (ISSN: 1096-0384)
Amano A; Aigaki T; Maruyama N; Ishigami A
In this study, we examined whether ascorbic acid (AA) and dehydroascorbic acid (DHA), the oxidized form of AA, levels in tissues regulate the AA transporters, sodium-dependent vitamin C transporters (SVCT) 1 and SVCT2 and DHA transporters, glucose transporter (GLUT) 1, GLUT3, GLUT4 mRNA by using senescence marker protein-30 (SMP30)/gluconolactonase (GNL) knockout (KO) mice.
¡¡
These mice are incapable of synthesizing AA in vivo. AA depletion enhanced SVCT1 and SVCT2 mRNA expression in the liver and SVCT1 and GLUT4 mRNA expression in the small intestine, but not in the cerebrum or kidney.
¡¡
Next, we examined the actual impact of AA uptake by using primary cultured hepatocytes from SMP30/GNL KO mice. In the AA-depleted hepatocytes from SMP30/GNL KO mice, AA uptake was significantly greater than in matched cultures from wild-type mice.
¡¡
These results strongly affirm that intracellular AA is an important regulator of SVCT1 and SVCT2 expression in the liver.
Ascorbic acid depletion enhances expression of the sodium-dependent vitamin C transporters, SVCT1 and SVCT2, and uptake of ascorbic acid in livers of SMP30/GNL knockout mice. https://reference.medscape.com/medline/abstract/20122894
¡¡
¡¡
¡¡
Dehydroascorbic Acid
¡¡
Pharmacology
Dehydroascorbic acid has similar biological activity as ascorbic acid. Both compounds have been shown to have antiviral effects against herpes simplex virus type 1, influenza virus type A and poliovirus type 1 with dehydroascorbic acid having the stronger effect. In addition, unlike ascorbic acid, dehydroascorbic acid can cross the blood brain barrier and is then converted to ascorbic acid to enable retention in the brain. This is important because one study has found that after an ischemic stroke, dehydroascorbic acid has neuroprotective effects by reducing infarct volume, neurological deficits, and mortality.
Mechanism of Action
Even though dehydroascorbic acid and ascorbic acid have similar effects, their mechanism of action seems to be different. The exact mechanism of action is still being investigated, but some have been elucidated. Concerning dehydroascorbic acid's antiviral effect against herpes simplex virus type 1, it is suggested that dehydroascorbic acid acts after replication of viral DNA and prevents the assembly of progeny virus particles.
Drug Indication
There is no approved indication for dehydroascorbic acid, but it has potential therapeutic use in patients with certain viruses and ischemic stroke.
Dehydroascorbic acid | C6H6O6 - PubChem https://pubchem.ncbi.nlm.nih.gov/compound/dehydroascorbic_acid#section=Top
¡¡
¡¡
¡¡
Photosensitized Oxidation of Ascorbic Acid in Urine and Blood Serum
¡¡
Mary L. Dodds Florence L. MacLeod Juanita Smith Carr
The Journal of Nutrition, Volume 32, Issue 5, 1 November 1946, Pages 559¨C565, https://doi.org/10.1093/jn/32.5.559
Published: 01 November 1946 Article history
¡¡
Summary
The photosensitized oxidation of reduced ascorbic acid in urine preserved at pH 2 to 3 has been shown to take place.
The ascorbic acid is present in the urine after oxidation as dehydroascorbic acid.
The reaction depends upon the presence of dissolved oxygen.
The reaction is accelerated by increasing amounts of riboflavin.
A loss of reduced ascorbic acid occurs in blood serum exposed to light.
¡¡
¡¡
Abstract : During a study of human requirements for ascorbic acid it was observed that reduced ascorbic acid in urine stored at pH 2 to 3 was destroyed on exposure to light. Total ascorbic acid was estimated by the method of Roe and Kuether (Abst. 261, Vol. 13) and reduced ascorbic acid by that of Evelyn, Malloy and Rosen (Abst. 4628, Vol. 8). Exposure of urine samples acidified with glacial acetic acid, to light from a tungsten-filament lamp caused less destruction of reduced ascorbic acid than exposure to skyshine of less intensity. Removal of oxygen from the urine by means of dry ice decreased, and addition of riboflavin accelerated, the destruction of reduced ascorbic acid.
¡¡
Experiments were made also with clear and haemolysed blood serum, analysed by the micromethod of Mindlin and Butler (Abst. 390, Vol. 8). Light from a 15 watt white fluorescent-light tube was as effective in causing oxidation of reduced ascorbic acid as light from a 300 watt tungstenfilament bulb. These findings suggested that loss of reduced ascorbic acid might occur in routine samples of urine and blood serum unless care was taken to guard them from light.-A. M. Copping.
https://www.cabdirect.org/cabdirect/abstract/19461404264
¡¡
Photosensitized Oxidation of Ascorbic Acid in Urine and Blood Serum | The Journal of Nutrition | Oxford Academic https://academic.oup.com/jn/article-abstract/32/5/559/4727124?redirectedFrom=fulltext
¡¡
¡¡
¡¡